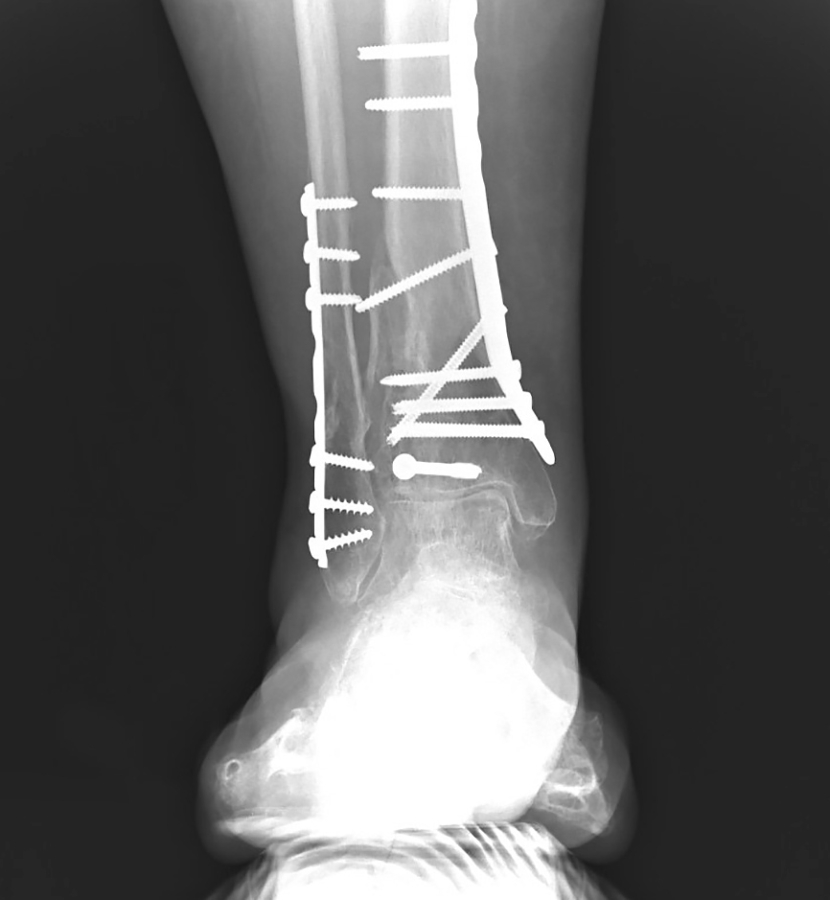
Tarsal coalition surgery
Restore your range of motion.
To repair abnormal connection across the foot’s bones and joints, Dr. Blitz performs tarsal coalition, talocalcaneal coalition, and calcaneonavicular coalition surgery through his Beverly Hills and NYC practices.